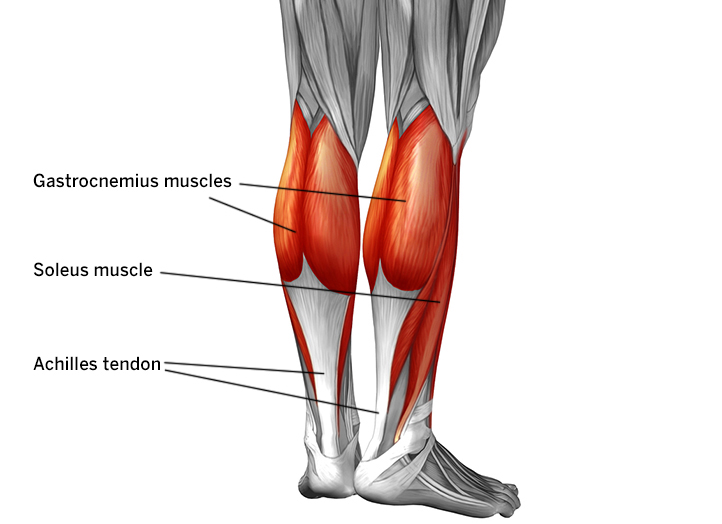
Achilles tendon is the biggest and strongest tendon in the human body. It attaches the calf muscle to the back of the heel. Its function is to transmit the forces of the calf muscle through to the foot facilitating movements such as walking, running, jumping and so on. However, it has relatively poor blood supply which results in poor healing rates post injury/trauma.
What is Achilles tendinopathy?
A tendinopathy is clinically described as a painful condition owing to overuse/increased loads on the tendon. Increased loads correlate to increased intensity of symptoms generally. The same is true for Achilles tendinopathy.
What are the types of Achilles tendinopathy?
The types are described based on the location of symptoms –
- mid-portion – affecting the intersection between the tendon and the gastrosoleus (calf) muscle
- nsertional – affecting the insertional portion of the tendon on the Calcaneal (heel) bone.
What are the signs and symptoms of Achilles tendinopathy?
- A combination of pain and morning stiffness in and around the Achilles tendon region is the single most common and a hallmark sign of Achilles tendinopathy.
- Pain and stiffness may decrease with initial return to activity but increase again with continuation of activity
If your symptoms do not fit this criteria, your condition may not necessarily by Achilles tendinopathy.
Other common conditions affecting the same region are:
- Sever’s disease (in adolescents)
- Posterior impingement syndrome
- Plantar fasciitis
A thorough assessment by your physiotherapist is the key to accurate diagnosis and treatment.
What are the causative factors?
- Achilles tendinopathy commonly affects active people, but inactive population is affected too. The biggest trigger to the condition is an unhealthy change in physical loads – such as increasing the distance/speed/frequency too soon.
- Not giving one’s body enough recovery in between sessions is a proven trigger too.
- Secondary to that, factors like obesity, Diabetes mellitus (type 1 & 2), hypercholesterolemia are also linked to Achilles tendinopathy.
What is the evidence based management strategy?
- The most important aspect of management is avoiding further irritation to the Achilles tendon by discontinuing/modifying the aggravating activities. For example, running can be replaced with cycling, swimming till the condition resolves.
- Once the tendon is irritated and is symptomatic, icing the area helps with settling the symptoms.
- Graded tendon loading/strengthening program remains the cornerstone for treatment of Achilles tendinopathy. However, this may take weeks to show results.
- A Physiotherapist can help multiple adjunct therapies for symptomatic relief in combination with the exercise therapy. They are:
- Shockwave therapy
- Dry-needling
- Soft tissue mobilisation/massage
- Strapping
- Optimal warm-ups and a gradual increase in physical loads are essential for the well-being of tendon. Your physiotherapist can help with a customised exercise program to tailor your needs.

